
Solving Healthcare's Biggest Challengeswith Workflow Automation
Healthcare organizations in the U.S. face mounting pressures from rising operational costs, labor shortages, and the increasing complexity of regulatory compliance. In fact, U.S. healthcare providers spend over $200 billion annually on administrative tasks, including billing, claims processing, and patient data management. Despite the critical importance of these tasks, many of these processes remain manual, time-consuming, and prone to errors.
In this blog, we’ll explore real-world examples of how workflow automation is improving efficiency and ROI for healthcare providers and payers, and why this technology is becoming essential for the future of healthcare operations.
The Challenges of Healthcare Operations: What’s Holding Us Back?
Healthcare operations in the United States face a perfect storm of challenges that are driving up costs, complicating workflows, and straining the ability to deliver quality care. The industry's landscape is increasingly burdened by rising operational expenses, complex regulatory requirements, and a shrinking labor force—each of which exacerbates inefficiency and reduces the capacity of healthcare organizations to perform at their best.
-
Rising Operational Costs
Healthcare costs in the U.S. are escalating at an unsustainable rate. In fact, U.S. healthcare spending has reached nearly $4.3 trillion, representing approximately 18% of the GDP. A significant portion of this spending is driven by administrative inefficiencies.
In 2023, a CAQH report estimated that healthcare organizations could save $13.3 billion annually by eliminating manual administrative tasks, such as billing and claims processing, which currently consume vast amounts of time and resources.
But the costs go beyond just administrative tasks. For instance, more than 35% of the average hospital’s operational budget is dedicated to staffing and payroll, with a large portion of that attributed to inefficient manual processes, which increase workloads and reduce staff productivity. These escalating expenses, coupled with a lack of effective automation, make it nearly impossible for healthcare organizations to stay financially sustainable in an environment of razor-thin margins.
-
Complex Regulatory Environment
As healthcare regulations become more stringent, the pressure on organizations to remain compliant is growing. In the U.S., the healthcare industry contends with over 600 regulatory requirements that span everything from data privacy laws (like HIPAA) to payer-specific billing codes and coding standards.
This complexity is compounded by the ever-changing nature of healthcare laws. Between 2017 and 2021, the Centers for Medicare & Medicaid Services (CMS) made over 200 updates to their rules alone, forcing healthcare providers and payers to adapt constantly. A recent survey of healthcare compliance professionals revealed that 58% of respondents cited regulatory complexity as one of their top challenges, making it increasingly difficult to keep up with the fast-paced changes in the regulatory environment.
Failure to stay compliant can be costly— penalties for non-compliance can amount to millions of dollars, and regulatory violations can severely damage an organization's reputation. Additionally, 15% of healthcare professionals report spending more than 20% of their time on compliance-related tasks, taking valuable time away from direct patient care and administrative efficiency.
-
Labor Shortages and Burnout
Perhaps the most immediate challenge facing healthcare organizations today is the growing shortage of skilled labor. The Bureau of Labor Statistics forecasts that the healthcare industry will need to fill more than 2.5 million new jobs by 2030 due to an aging population and increased demand for healthcare services. This includes shortages of physicians, nurses, medical technicians, and administrative staff.
Labor shortages are directly linked to the burnout crisis in healthcare. A 2023 survey by the American Medical Association revealed that 63% of healthcare workers are experiencing burnout, with more than 40% of healthcare professionals considering leaving their roles due to stress, fatigue, and workload pressure. In particular, hospital administrators report that staffing shortages are leading to increased workloads for remaining staff, affecting the quality of care and creating a vicious cycle of inefficiency.
One factor contributing to this burnout is the manual, repetitive tasks that many healthcare workers still handle on a daily basis. From data entry to claim processing, many of these tasks are draining valuable time and energy from healthcare professionals, preventing them from focusing on more meaningful work that drives patient care.
-
The Compounding Effect of These Challenges
Together, rising operational costs, regulatory complexity, and labor shortages create a perfect storm for inefficiencies in healthcare. Studies show that U.S. healthcare providers spend upwards of 16 hours per week on administrative tasks alone, much of which could be automated, freeing up valuable time for both clinical and non-clinical staff.
As these pressures continue to mount, the need for comprehensive solutions to streamline workflows, reduce errors, and enhance compliance becomes more critical than ever. Healthcare organizations cannot afford to ignore the mounting costs of inefficiency, and the path forward will likely depend on their ability to leverage technology—particularly automation—at scale. The future of healthcare hinges on the industry’s ability to adapt to these challenges and find smarter, more efficient ways to deliver care.
-
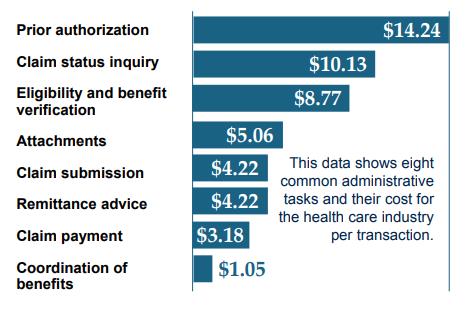
CAQH Study Provides Insight into Projected Cost Benefits
In a recent study, the Council for Affordable Quality Healthcare (CAQH) found the health care industry could save $13.3 billion if eight administrative tasks in the revenue cycle were no longer completed manually. 7 Revenue cycle automation is one of the many applications where workflow automation can play a pivotal role.
RELATED: A Guide to Healthcare IT Compliance
The ROI of Automation: Turning Challenges into Opportunities
Workflow automation can assist both clinical and non-clinical stakeholders in care delivery by enhancing performance on cognitive tasks, allowing for more efficient decision-making and improved outcomes.
Leveraging automation in healthcare can:
- Reduce unnecessary variance by standardizing workflows across specialties, practices, and regions, ensuring consistency in care delivery. According to a study in the Journal of the American Medical Association (JAMA), hospitals that implemented standardized care protocols saw a 30% reduction in readmission rates and 20% improvement in patient outcomes. By reducing clinical variability, patients receive more consistent, evidence-based care.
- Increase access to healthcare services by removing physical and administrative barriers, making it easier for patients to receive timely care.
- Improve safety and healthcare outcomes by ensuring adherence to evidence-based safety protocols and reducing human error, enhancing patient safety.
- Boost productivity for clinical and non-clinical workers by automating repetitive tasks, allowing more time for direct patient care and management.
- Enhance decision-making by providing real-time, data-driven insights to clinicians, enabling faster and more accurate diagnoses and treatments.
- Support regulatory compliance by automating updates and checks to align with the latest healthcare standards, reducing the risk of non-compliance. According to a Deloitte report, automating compliance processes can reduce the risk of errors by up to 40% in claims processing and compliance checks.
- Reduce operational costs by streamlining administrative tasks, reducing overhead, and increasing operational efficiency. For example, the Cigna Healthcare automated their claims adjudication process, reducing manual intervention and decreasing claims processing time by 20%.
- Improve patient satisfaction by speeding up processes like appointment scheduling, billing, and claims processing, leading to a smoother patient experience.
Automation has already made strides in certain areas of healthcare, particularly in administrative and operational tasks. However, the industry has yet to fully realize its potential. While many routine processes have been automated, workflows that require human judgment and decision-making have seen less automation.
Success in Action: Real-World KPi Use Cases of Healthcare Automation
Here are a few use cases for workflow automation in healthcare based on KPi-Tech's case studies:
- Automating Healthcare Data Validation: KPi-Tech helped a healthcare provider automate their data validation processes, resulting in a 96% reduction in validation time. By implementing an automated system, the organization streamlined its operations, reducing manual errors and improving overall data accuracy, enabling quicker decision-making.
- Automating Payer Risk Contract Management: In a women's healthcare network, KPi-Tech automated the management of payer risk contracts. This solution helped the organization manage contracts more efficiently, ensuring accurate eligibility assessments and reducing administrative overhead. It enabled faster decision-making and improved the management of risk contracts for eligible patients.
- Streamlining SOP Management: KPi-Tech developed an AI-powered chatbot for a pharmaceutical client to streamline over 500 standard operating procedures (SOPs). The automation allowed the organization to boost efficiency, reduce human error, and facilitate faster, more informed decision-making within the operations.
- Automating Integration Verification: KPi-Tech developed an automated solution for multi-client healthcare integration verification. This improved the validation process, reducing the time spent on verification tasks by 96%. The solution enhanced overall efficiency and helped ensure smoother data exchanges between healthcare systems.
- Automating PBM Enrollment and Claims Management: KPi-Tech helped a self-insured healthcare provider automate the enrollment process for Pharmacy Benefits Manager (PBM) and streamline claims management. By implementing automation, the organization reduced the manual effort involved in enrolling members and processing PBM claims. This led to faster claims resolution, fewer errors, and improved member satisfaction. Automation also ensured better compliance with PBM-specific regulations and reduced administrative costs.
- CRM Automation Testing for Faster Onboarding: KPi-Tech helped a healthcare data analytics company optimize their CRM implementation by automating the Quality Assurance (QA) testing process. By integrating automation into the testing workflow, the company reduced testing time by 93%. This automation led to 15x faster onboarding of new clients, enabling the organization to scale operations more efficiently. The quicker testing cycle also improved the reliability of the CRM system, ensuring better data management and enhanced client satisfaction, ultimately driving a higher return on investment (ROI).
RELATED: How Healthcare Automation Can Enhance Efficiency, Interoperability, and Patient Care?
Conclusion
The promise of workflow automation in healthcare isn’t just about technology—it’s about transformation. By starting with small, impactful changes in repetitive and error-prone tasks, the healthcare industry can chip away at inefficiencies that have long burdened providers and payers. True success lies in aligning stakeholders around a shared vision of streamlined care delivery. While the path to full automation may be gradual, each step brings us closer to a system where quality, safety, and provider well-being are no longer compromised by outdated workflows. It’s not just about solving today’s problems—it’s about building a smarter, more sustainable future for healthcare.
Unlock the Power of Workflow Automation with KPi-Tech
At KPi-Tech, we understand that navigating the complex healthcare landscape requires innovative solutions that drive efficiency and improve patient care. Our tailored workflow automation solutions are designed to streamline your operations, reduce administrative costs, and enhance regulatory compliance—all while improving patient satisfaction and outcomes.
Whether you're looking to automate claims management, optimize PBM enrollment, or enhance data validation, we have the expertise and proven track record to help your organization achieve measurable improvements. Our approach is built on real-world success stories and cutting-edge technology to ensure seamless integration and maximum ROI.





